Are you suffering from chronic back pain? Do you want an effective solution that helps you get rid of your prolonged pain?
If so, it’s time to consider radiofrequency neuroablation!
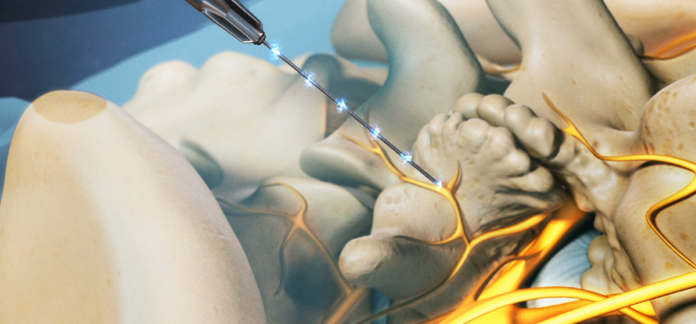
Pain relief is achieved using radiofrequency ablation (or RFA). A small portion of nerve tissue gets heated by a radio wave’s electrical current, which reduces the pain signals from that region.
The most typical indications for radiofrequency neurotomy include back, neck, and buttock pain (sacroiliac joint). It may also benefit long-term joint pain in the shoulder, knee, or hip.
Why is it Performed?
The person doing radiofrequency neuroablation is typically a pain management specialist. When medication, physical therapy, or surgery are not options, the aim is to lessen persistent back, neck, hip, or knee pain.
When you have back discomfort, for instance, your doctor might advise the following procedure:
• Takes place on one or both of your lower back sides.
• Spreads to the thighs and buttocks (but not below the knee)
• When you twist or lift something, it hurts more.
• When you’re lying down, it feels better.
What Happens During Treatment?
You will be required to sign consent paperwork, identify any current drugs you are taking, and state whether you have any pharmaceutical allergies at the time of the treatment. After the quick operation, there may be a 15–45 minute recuperation period.
Step 1: Prepare the Patient
On an x-ray table, the patient is lying down. The treatment region is numbed with a local anesthetic. The technique causes the patient just minor discomfort. Throughout the procedure, the patient is awake and conscious and can offer comments to the doctor. Typically, only a low-dose sedative—like Valium or Versed—is administered during this treatment.
Step 2: Insert the Needle.
The method utilized for diagnostic blocks is identical to that used for nerve ablation. The doctor inserts a tiny hollow needle into the area causing the pain using a fluoroscope, a special x-ray. To ensure that the needle is inserted into the intended spot, the doctor can use fluoroscopy to watch the needle in real-time on the fluoroscope monitor. Contrast may be administered to ensure the needle is in the right place. There is some discomfort, but for most people, pressure overlies pain.
Step 3: Deliver Heating Current.
The patient is given an anesthetic after the needle is inserted. The hollow needle is then subjected to a radiofrequency current to produce a lesion, a tiny burn roughly the size of a cotton swab tip. The pain-transmitting part of the nerve is destroyed by the current, which also distorts the signal that causes the pain. Each burn site takes around 90 seconds to complete and may burn several nerves simultaneously.
Depending on the treatment site and the number of treatments administered, radiofrequency ablation can be finished in 15 minutes to two hours.
What are the side effects and risks of radiofrequency ablation (RFA)?
Similar to what you felt before the operation, you might feel some discomfort or a burning sensation on the spot during it. Following the treatment, the pain could last for a week or more. You can reduce the pain by placing an ice pack in the area and applying it for 20 minutes intermittently.
When the needle is inserted into your skin, you can experience momentary numbness.
Complications from RFA are extremely unlikely. Pain or irreversible nerve injury might happen occasionally.
Conclusion
The radiofrequency ablation process is generally low-risk and safe. However, this treatment may have certain adverse effects and difficulties for some patients. Before beginning RFA, it is important to talk with a doctor about the potential risk of experiencing any negative reactions or side effects.
—————————————-